“Pfizer’s phony rhetoric.”
The free market? Let us count the public money behind its vaccine.
So much for the idea that governments shouldn’t be in the business of picking winners and losers. We are now on the threshold of achieving the first effective vaccine for a coronavirus—this in record time. Despite protests to the contrary, good government policy can actively shape good outcomes that benefit society.
This new reality at an urgent moment has implications well beyond Covid–19 and should inform our broader policy choices going forward in healthcare and overall national development. What is the role of the state? You’re not going to get an honest or intelligent answer to this very vital question out of Pfizer, one of Big Pharma’s heaviest hitters: You’re going to get Friedmanesque ideology and hypocrisy: This is among the week’s essential lessons.
It has been a good week, certainly, for those looking for a light at the end of the dark Covid–19 tunnel: We now have interim data from two well-run vaccine trials suggesting exceptionally high thresholds of effectiveness—in excess of 90 percent—first from the Pfizer–BioNTech consortium and this week from Moderna. The euphoria was understandable, given that most public health officials had expected any new vaccine to be 60 percent to 70 percent effective. (The Food and Drug Administration had established a 50 percent threshold to secure regulatory approval for distribution.) As with any new vaccines, it will take time to determine the vaccines’ longer-term efficacy in terms of sustaining immunity, especially given the revolutionary technologies that underline them.
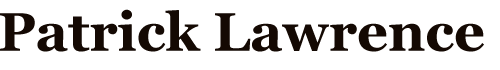
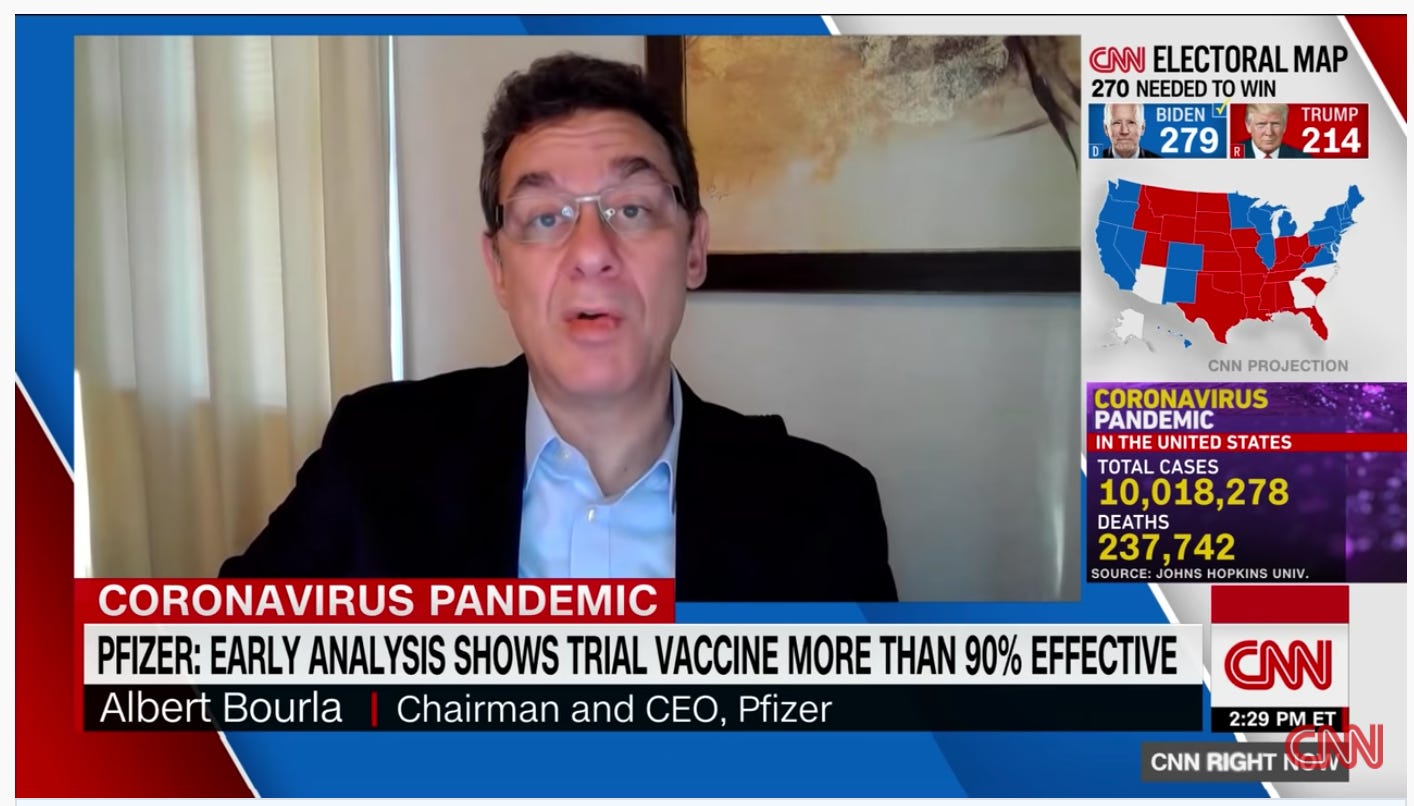
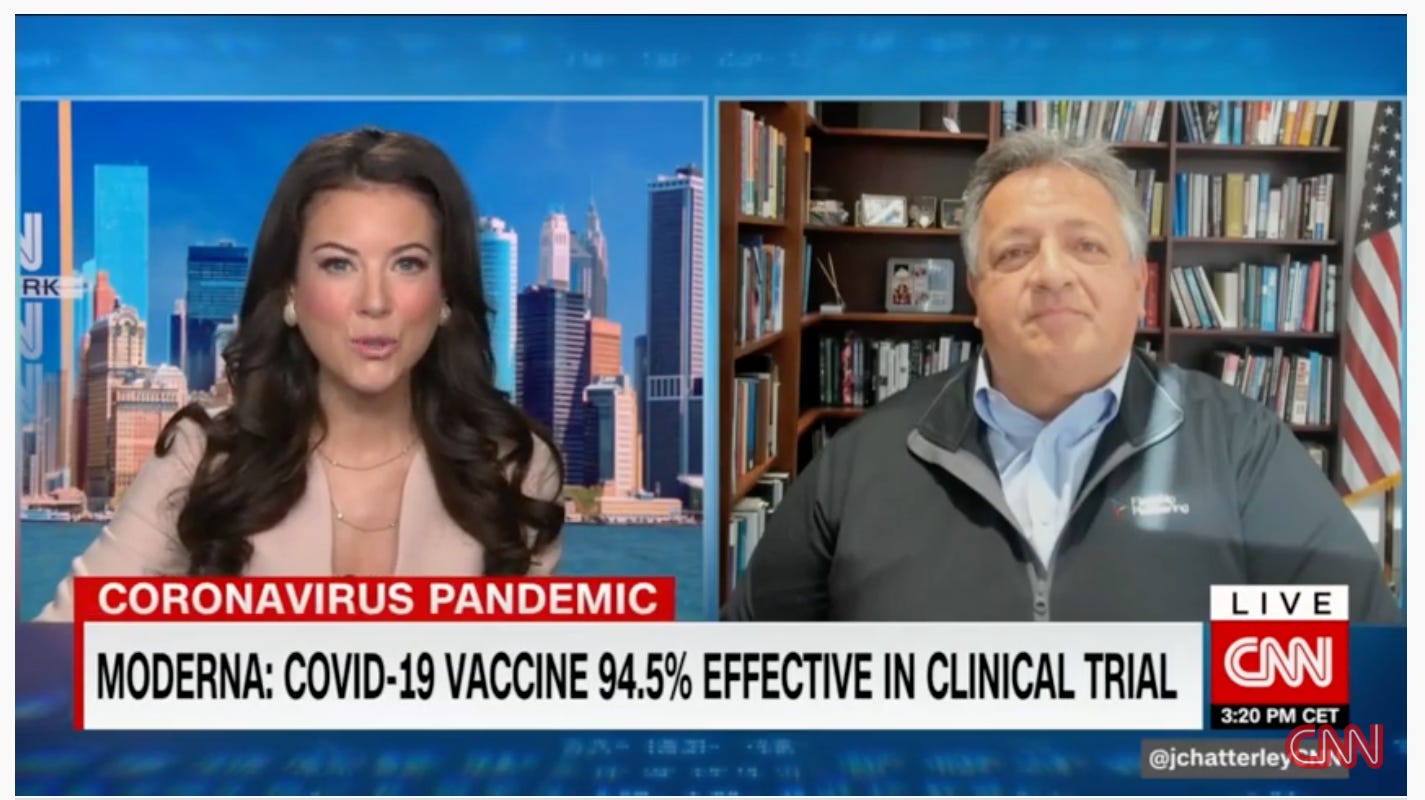
Yet it was interesting to note the contrasting statements put out by the chief execs of Pfizer and Moderna, Albert Bourla and Stephane Bancel respectively, when each announced successful Phase 3 interim results. Moderna’s CEO graciously praised and comprehensively acknowledged the role played by the U.S. government, specifically the National Institutes of Health, the Biomedical Advanced Research and Development Authority and, equally significant, “Operation Warp Speed,” the public-private program initiated by the Trump administration to accelerate the development, manufacture, and distribution of Covid–19 vaccines. By contrast, Pfizer’s CEO went out of his way to let us know that his company’s potentially game-changing research and development was funded without any direct U.S. government assistance. His rationale for not accepting public R&D funding was as follows:
The reason why I did it was because I wanted to liberate our scientists from any bureaucracy…When you get money from someone that always comes with strings. They want to see how we are going to progress, what type of moves you are going to do. They want reports. I didn’t want to have any of that. I wanted them — basically I gave them an open checkbook so that they can worry only about scientific challenges, not anything else.
In other words, no meddling government bureaucrats with their Gosplan centralized planning instincts to jeopardize the development of a game-changing vaccine.
There’s lot to unpack here, but to put it charitably the Pfizer chief executive is being somewhat economical with the truth. Big Pharma’s most profitable global market by far is the United States, largely because of its government’s reticence to curb drug price increases. Albert Bourla has every incentive to maintain this happy state of affairs. Giving any credit to a private-public joint venture would undoubtedly raise some uncomfortable questions about the country’s for-profit healthcare system, even though, as the economist Mariana Mazzucato has highlighted, “the NIH invests some $40 billion a year on medical research and has been a key funder of the research and development of Covid–19 treatments and vaccines.”
This is a factor that Stephane Bancel had little compunction in recognizing, which is only fair considering that Moderna, a much smaller biotechnology company, accepted nearly $1 billion in research aid from Uncle Sam, along with a further $1.5 billion to take a supply order from the federal government—this well before anybody had any idea whether the drug trials would succeed. In fact, the contributions from the U.S. (and other governments) helped Moderna to turn cash flow positive in the third quarter this year for the first time in its 10–year history.
Certainly, nobody seems to be complaining too loudly about the government being in the business of picking winners and losers today: Moderna’s late-stage vaccine trials showed that it was 94.5 percent effective in preventing the disease and, requiring only refrigeration as against very deep freezing, easier to transport and store than the Pfizer product. Maybe there is something to be said for public-private partnerships after all.
In spite of Moderna’s success, it is noteworthy that Bourla’s paean of praise to the free market has been swallowed hook, line, and sinker in a variety of publications, even though it is misleading in several respects:
¶ Pfizer did take significant funds from the US government to the tune of $1.95billion for up to 600 million doses. It went this way: Taxpayer money went toward future distribution of Pfizer’s vaccine, not research. O.K., Pfizer can claim it didn’t depend on the public sector to finance its R&D. But look more closely: This whack of dough freed up additional capital to help Pfizer fund the R&D. This looks like a distinction without a difference to me.
Pfizer certainly didn’t think it was chump change last summer, when it gratefully accepted nearly $2 billion in public funding. And now it churlishly seeks to distance itself from “Operation Warp Speed.” Nonsense, to put it mildly.
¶ Even if Pfizer didn’t receive any direct R&D funding from the U.S.government, its German partner, BioNTech SE, did receive public funding: It got $445 million from the Federal Republic. The significance here is that BioNTech was specifically credited with the development of the revolutionary technology behind the vaccine, the so-called messenger RNA, or mRNA.
That is a process whereby a genetically designed script, in effect a lab-created DNA instruction manual, is injected into the patient, prompting the body to make viral proteins to engender an immune response to the virus. It differs from the traditional approach to vaccine development, whereby an actual fragment of a virus is used to generate the immune response (a more traditional method being used by the Oxford University–AstraZeneca consortium, among others).
Given the historically close collaboration between Pfizer and BioNTech—they have worked together for more than two years—it beggars belief to suggest that Pfizer didn’t derive significant benefits from its German partner’s contribution to the overall project (and, by extension, the German government’s funding assistance on the R&D). mRNA is a game-changing technology that, if successful, could enhance future pandemic mitigation against comparable coronaviruses, because it offers the potential to modify the mRNA genetic scripts to deliver a successful immune response if and when newer virus strains emerge in the future.
Where is Bourla’s storyline now? Where. Dr. Bourla, are your overweening Berlin bureaucrats demanding quotas, targets, and endless reports that would have interfered with this groundbreaking achievement? The man spouts free-market ideology and then accepts assistance at one remove from a social-democratic government. Hmmm.
And guess what. Private investors also like to get information as to how their money is going to be spent—and this means progress reports, drug updates, targets, etc. Indeed, in some respects, private investors are even more difficult than governments: They demand information on a quarterly basis, often pressuring management to deploy cash flow in way that is less consistent with long research and development and more aligned to short-term considerations like beating a quarterly earnings estimate by Wall Street, or securing a higher dividend payout: That’s the legacy of Milton Friedman’s pernicious doctrine of “shareholder capitalism.”
Free-market fictions.
Why would Pfizer go out of its way to minimize the government’s contribution? Part of this is likely the toxicity associated with the Trump administration, even though Operation Warp Speed itself appears to have been a conspicuously successful public-private collaboration. This is the fastest any new vaccine has ever been developed. Further, there are other drugs in the pipeline from companies that did accept U.S. government funding for R&D purposes. Despite that success, there has been a concern that the U.S. president’s involvement politicized the science behind the vaccine and thereby undermined the drug companies’ ability to secure widespread acceptance for the new drugs.
A political campaign season is hardly a good backdrop for a rational discussion of scientific policy at the best of times, let alone our recent spectacle. But Trump has now lost the election. As the U.S. looks toward a new administration, Pfizer’s CEO must have other objectives in mind as he dismisses the public sector and pretends to go it alone. Let us think this through.
It is likely that part of the Pfizer game plan is to pre-empt any discussion of how we handle drug procurement in the U.S., which is unique among developed economies for the exorbitant prices we pay for pharmaceutical drugs. Even though Joe Biden explicitly campaigned against Medicare for All, he is on record as calling for an expanded public option for what’s left of the Affordable Care Act, which in theory could put some of Big Pharma’s profit margins under pressure.
Anything that smacks of the government using its monopsony power to lower drug prices (as has been done in virtually every other Western nation) naturally creates anxiety in America’s privately run pharmaceutical complex. In U.S. health care, the free market fundamentalists remain ideologically fixated on the idea that the answer to predatory pricing is more competition. That can’t happen in an environment where a government encourages oligopolies and refuses to use its considerable purchasing power to determine pricing.
Whenever significant number of politicians (normally Democrats) have called for the government to exercise this power via programs such as Medicare for All, the leading powers of the healthcare system—Big Pharma and the private health insurance industry—quickly mobilize opposition in Congress (to whom they have generously donated precisely for this purpose), much as Wall Street banks thwarted wholesale financial reform in the wake of the 2008 crisis, even when those banks were at death’s door.
The standard rationale proffered by Big Pharma companies such as Pfizer when confronted with the reality of high U.S. drug prices is that drug research and development is a very expensive and highly uncertain endeavor; hence, pharmaceutical companies must generate substantial profits to finance this innovation process. However, like many of their counterparts in other industries, U.S. pharmaceutical companies have been increasingly deploying their substantial profits not toward R&D, but share buybacks, which undermines the justification for the exorbitant prices of their products.
Big Pharma’s other rationale for high prices—namely, to recoup the amount of time and cost deployed toward the research undertaken—conveniently ignores the fact that many of their “pioneer” drugs were originally devised in academic laboratories with considerable federal government support, only then to be patented and licensed to private companies. Former Congressman Henry Waxman got this down on paper in a 2017 report, “Getting to the Root of High Prescription Drug Prices: Drivers and Potential Solutions.”
In fact, a number of innovative developments in health care treatments have arisen in countries that do tightly constrain costs, such as France and Switzerland, while still sustaining a number of thriving privately run pharmaceutical companies. Switzerland’s Roche and France’s Sanofi are two such examples. All of which undermines the “free rider” argument often trotted out by Big Pharma when questioned as to why foreign countries’ drug prices are so much lower than American prices. Furthermore, as the Commonwealth Fund has illustrated, the lack of price controls hasn’t exactly given the United States a massive qualitative edge in health care provision:
1. The U.S. ranked last place among the 11 countries for health outcomes, equity, and quality, despite having the highest per capita health earnings.
2. The U.S. also had the highest rate of mortality amenable to healthcare, meaning more Americans die from poor care quality than any other country involved in the study.
3. Poor access to primary care in the U.S. has contributed to inadequate chronic disease prevention and management, delayed diagnoses and safety concerns, among other issues.
All of which suggests that creating innovative ways of manufacturing a new drug product at scale best left to the devices of the free market, is a fallacy. Pfizer’s CEO is making the case for a large and increasingly discredited notion of free-market fundamentalism that eschews any role for government, other than to protect property rights (especially Big Pharma’s lucrative intellectual property rights), as well as creating and sustaining efficient, rent-free markets.
NIH funding and Operation Warp Speed have put us on the threshold of developing an effective vaccine to wipe out a dangerous pandemic in record-setting time. Moderna’s CEO at least had the good grace to acknowledge that absent significant government support, it is most unlikely that we would have had this kind of success so quickly. In fact, Modern might otherwise not even be alive today.
Of course, acknowledging a positive role for government calls into question many longstanding shibboleths about U.S. healthcare, as well as calling into question the pernicious myth peddled for decades that governments ought to play no national developmental role in the economy. In the specific case of Covid–19, such an acknowledgment would legitimize the heretical notion that medicines developed with government assistance should give the public sector a say in how these drugs are priced. Best to nip those dangerous ideas in the bud. Consider Dr. Bourla’s messaging in that context; it represents a pre-emptive attack on any attempts to change America’s comfortable healthcare status quo for Big Pharma.